Keratoconus : diagnosis and treatment
Keratoconus is a progressive eye condition where the normally round cornea thins and begins to bulge into a cone-like shape. This abnormal shape causes visual distortion as light entering the eye is refracted improperly. The condition often begins in the teenage years and can progress into the 30s or 40s.
Causes of Keratoconus
The exact cause of keratoconus is still not fully understood, but it is believed to be a combination of genetic and environmental factors. Here are some key contributors:
Genetics: A family history of keratoconus can increase the risk, suggesting a genetic predisposition.
Eye Rubbing: Vigorous or chronic eye rubbing has been associated with the progression of keratoconus, possibly due to the mechanical stress on the cornea.
Underlying Conditions: Certain systemic conditions, such as connective tissue disorders, may also be linked to a higher likelihood of developing keratoconus.
Symptoms of Keratoconus
Keratoconus can present with a variety of symptoms, typically worsening as the condition progresses:
Blurred or Distorted Vision: As the cornea changes shape, it leads to a noticeable decline in the quality of vision.
Increased Sensitivity to Light: Bright lights can become uncomfortable and may cause glare or halos.
Frequent Prescription Changes: Patients may notice their glasses or contact lens prescription changes frequently.
Double Vision: Especially in one eye, known as monocular diplopia.
How Common is Keratoconus?
Globally, keratoconus affects approximately 1 in 2,000 people. However, the prevalence can vary based on population and diagnostic criteria.
In Australia, studies suggest that the prevalence of keratoconus in some areas may be as high as 1 in 84 ( based on recent data from the Raine Study, which utilized Scheimpflug imaging) - much higher than the global average. This suggests that keratoconus may be more common in Australia than previously thought.
Diagnosis of Keratoconus
During a routine eye exam, an optometrist or ophthalmologist may notice irregular astigmatism, which could prompt further investigation. Key diagnostic tools include corneal topography, which maps the shape of the cornea.
An advanced method found in clinics specialising in keratoconus is Scheimpflug imaging (e.g. Pentacam scan), which provides detailed, three-dimensional images of the cornea's structure, allowing the earliest signs of keratoconus to be detected and monitored. It can detect keratoconus before any symptoms appear, and is more sensitive than corneal topography.
Treatment Options for Keratoconus
Managing keratoconus depends on the severity of the condition, and several options are available:
Glasses and Soft Contact Lenses:
In the early stages of keratoconus, vision can often be corrected with glasses or soft contact lenses. However, as the cornea becomes more irregular, these options may no longer provide adequate vision correction.
Rigid Gas Permeable (RGP) Corneal Lenses:
As keratoconus progresses, rigid gas permeable lenses are often recommended. These lenses are smaller and sit directly on the cornea, providing a new, smooth refracting surface that compensates for the irregular shape of the cornea.
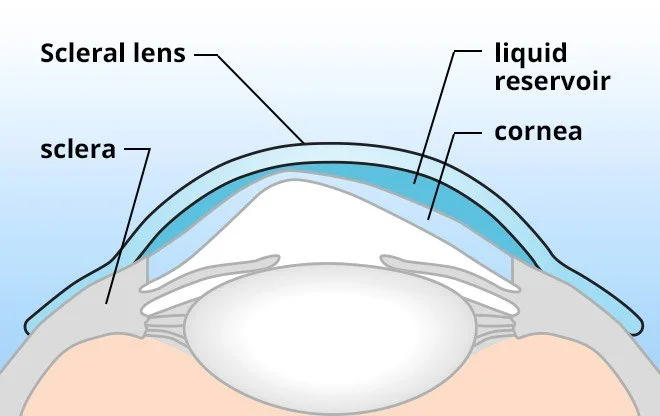
Scleral Lenses:
Scleral lenses are larger than traditional RGP lenses and rest on the sclera (the white part of the eye) rather than the cornea. Because they vault over the entire cornea, scleral lenses are particularly beneficial for advanced keratoconus where the corneal shape is highly irregular. The space between the lens and the cornea is filled with a saline solution, providing comfort and improving vision by creating a smooth optical surface.
Scleral contact lens for keratoconus
Scleral lens for keratoconus and corneal grafts
Corneal Cross-Linking (CXL):
This minimally invasive procedure uses riboflavin (vitamin B2) and ultraviolet light to strengthen corneal tissue, helping to halt the progression of keratoconus. While CXL does not reverse the condition, it can stabilize the cornea and prevent further deterioration.
Corneal Graft
In severe cases, when other treatments are no longer effective, a corneal graft / transplant may be necessary. This procedure involves replacing the damaged cornea with a donor cornea.
Related Conditions
Keratoconus is often associated with other conditions, which may share common underlying mechanisms or risk factors:
Vernal Keratoconjunctivitis: A type of allergic eye disease that causes severe itching, which can lead to eye rubbing and possibly contribute to keratoconus.
Down Syndrome: Individuals with Down Syndrome are at a much higher risk of developing keratoconus, possibly due to a combination of genetic and environmental factors.
Atopic Conditions: Conditions such as asthma, eczema, and hay fever, which are associated with allergies and frequent eye rubbing, have also been linked to keratoconus.
Eye rubbing
In patients with keratoconus, eye rubbing can accelerate the progression of the disease by making the cornea more irregular in shape.
If you suffer from allergies, rubbing your eyes can make your symptoms worse by releasing more histamines, which increases itchiness, redness, and irritation, making you want to rub your eyes even more. This creates a harmful cycle that can lead to further corneal damage.
If allergies are a problem, your optometrist may prescribe antihistamine drops (such as Zaditen or Patanol) or oral allergy meds.
Common questions
Can Keratoconus be cured?
Keratoconus cannot be cured, but its progression can be managed effectively with treatments. Corneal cross-linking (CXL) is the most common procedure to halt the progression of keratoconus by strengthening the cornea. While treatments like specialized contact lenses and corneal transplants can improve vision and quality of life, they don't reverse the underlying condition
Does Keratoconus Increase with Age?
Keratoconus typically begins in adolescence and progresses into the early adult years. The progression of keratoconus generally slows down with age, particularly after the 40s. By this age, the cornea tends to stabilize, and further significant changes in corneal shape are less likely.
Does Screen Time Worsen Keratoconus?
There is no direct evidence to suggest that screen time worsens keratoconus.
Can Keratoconus Cause Blindness?
Keratoconus itself does not directly cause blindness. However, in severe cases, the corneal thinning and distortion can lead to significant vision loss. If left untreated, keratoconus can severely impair vision, but with modern management options, such as corneal cross-linking and advanced contact lens designs, most patients can maintain functional vision. In the most advanced cases, where corneal scarring occurs, a corneal transplant may be necessary to restore vision.
Conclusion
While keratoconus can cause significant visual impairment if left untreated, modern treatments offer effective ways to manage the condition and prevent severe vision loss. More advanced keratoconus may require optometric management with specialty contact lenses, or ophthalmological management with crosslinking and corneal transplants.
In our practice we regularly manage patients with keratoconus and corneal grafts- often with corneal RGPs or scleral contact lenses. These patients are often referred to us by ophthalmologists or other optometrists.
Author Bio
Jenny Wu is an optometrist based in Canberra, Australia. She is a full scope optometrist specializing in dry eye, specialty contact lenses, myopia control, and orthok. She practices at Simpson Optometry. In her spare time she enjoys spending time in nature, photography, gardening, and being with her husband (also an optometrist) and 2 children.
Millodot, M., et al. "Prevalence and associated factors of keratoconus in Jerusalem: a cross-sectional study." Ophthalmic and Physiological Optics, 2011.
Wollensak, G., Spoerl, E., & Seiler, T. "Riboflavin/ultraviolet-A-induced collagen crosslinking for the treatment of keratoconus." American Journal of Ophthalmology, 2003.
Sahebjada, S., et al. "Prevalence of Keratoconus Based on Scheimpflug Imaging: The Raine Study." Ophthalmology, 2020.